Understanding Dental Implant Cost: A Guide to Risk and Decision Clarity
The Architecture of Choice: Understanding Dental Implant Cost
When you begin researching dental implant cost, you are likely looking for a definitive anchor—a specific number that signals you are making a “fair” or “correct” deal. It is a logical starting point for any significant investment. However, the surface-level quest for a price list often masks a deeper, unspoken fear: the fear of permanent regret.
The hidden anxiety isn’t just about the dollar amount; it is the worry that you might pay a premium for a result that fails, or conversely, choose a lower-cost option only to find it leads to a lifetime of corrective procedures. In high-stakes dentistry, the search for a “correct” price is often a search for a guarantee that doesn’t exist in a vacuum.
Why Price Transparency Feels Impossible
The confusion surrounding dental implant cost exists because the dental industry sits at a strange intersection of retail and complex medicine. We are conditioned to shop for products—like cars or electronics—where features can be compared side-by-side. Naturally, we try to apply this same logic to our health.
When faced with the vast variance in quotes, shortcuts become incredibly tempting. You may find yourself focusing on:
-
Specific Brands: Assuming the hardware manufacturer is the primary driver of success.
-
Speed: Valuing “immediate” results because they reduce the time spent in uncertainty.
-
Rankings: Looking for “top-rated” lists to outsource the difficult work of clinical vetting.
These shortcuts feel like safety nets, but they often ignore the most important variable: your unique biological landscape. When the focus stays on the “number,” the actual complexity of the procedure is obscured, leading to the primary objection: “I might waste my money on a choice I can’t undo.”
Reframing the False Belief: Cost as Risk Management

The belief that there is a “correct” or standard dental implant cost persists because we view the implant as a commodity—a piece of hardware you “buy.” In reality, a dental implant is a clinical outcome you facilitate.
To regain clarity, it is helpful to replace the “fixed price” mindset with a Risk Management Model. In this framework, the cost is not a random number; it is a reflection of the resources required to eliminate variables that could lead to failure. When you see a higher quote, you aren’t necessarily paying for a “fancier” screw; you are likely looking at a different level of risk mitigation:
-
Diagnostic Precision: Moving from 2D X-rays to 3D Cone Beam CT scans to map nerve pathways and bone density.
-
Structural Foundation: The difference between placing an implant in healthy bone versus recreating bone through grafting to ensure long-term stability.
-
Component Synergy: Ensuring the crown, abutment, and screw are engineered to distribute biting forces without fatiguing the metal.
Decision Scenarios: Mapping Your Context
Understanding your specific context helps move the conversation from “How much?” to “What is being managed?”
-
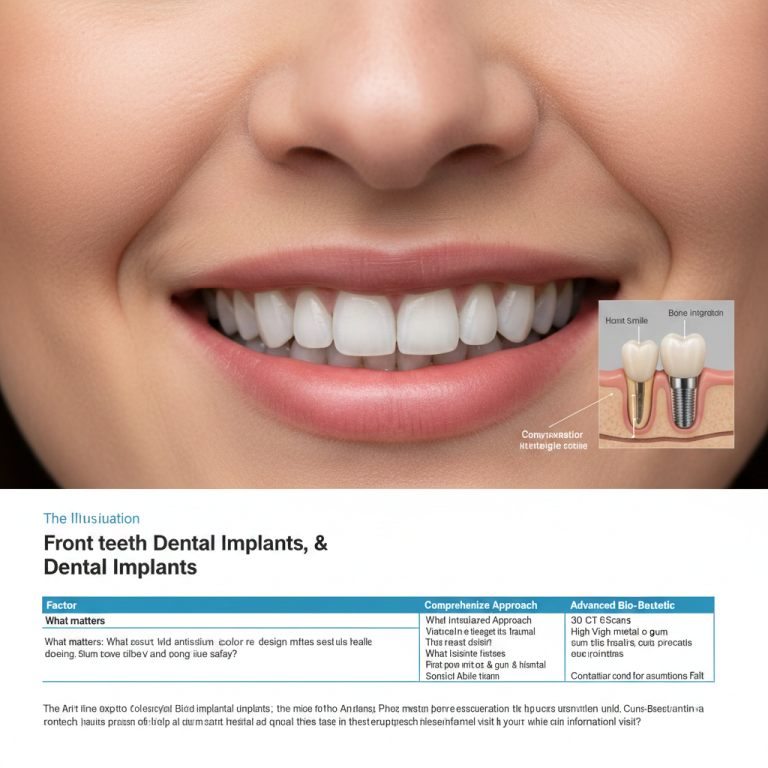
The Single Tooth “Smile Zone” Case: The missing tooth is in the front. What matters: Perfect aesthetic integration and gum-line symmetry. The worry: That the final result will look artificial or the metal will show through the tissue over time.
-
The Functional Molar Case: The missing tooth is in the back. What matters: Mechanical endurance and the ability to chew high-density foods. The worry: That the implant will fracture or loosen under the heavy pressure of the posterior jaw.
-
The High-Risk Medical Profile: The reader has underlying conditions like a history of bone loss or smoking. What matters: Biological integration and infection control. The worry: That the body will reject the implant regardless of the price paid.
Context Comparison: Planning for Predictability
This table outlines how different procedural philosophies manage variables. It is designed to help you identify which level of planning matches your personal tolerance for risk.
| Factor | Standardized Approach | Comprehensive Planning | Advanced Bio-Guided Planning |
| Decision Certainty | Moderate; relies on average healing | High; uses patient-specific data | Very High; addresses specific deficits |
| Long-term Predictability | Variable based on lifestyle | High stability over decades | Highest; designed for high-risk profiles |
| Planning Complexity | Routine diagnostics | 3D imaging & digital design | Multi-stage tissue/bone architecture |
| Risk if Assumptions Fail | Revision surgery may be needed | Minimal; risks identified early | Near-zero; contingencies built-in |
| Flexibility Over Time | May require specific parts | Usually compatible with major systems | Fully modular for future life changes |
The “Maintenance” Variable: Protecting Your Integration

When evaluating dental implant cost, recognize that the investment extends beyond the day of surgery. A significant portion of a comprehensive quote often accounts for the long-term “warranty” of biological integration.
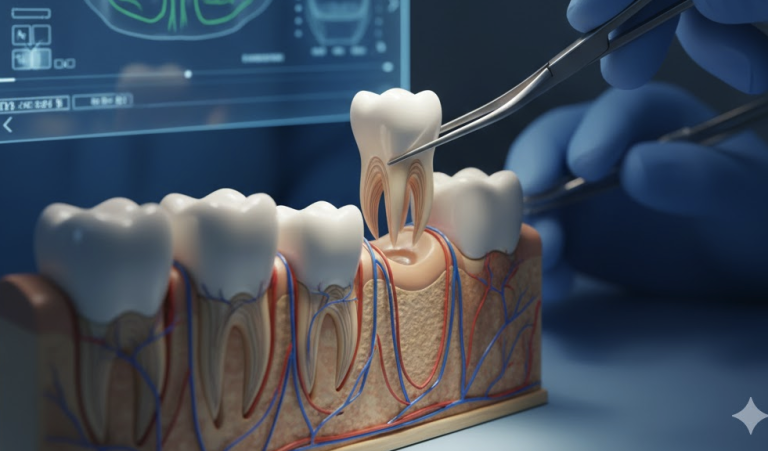
An implant must function within a living, changing environment. The initial cost often includes the clinical resources required to monitor osseointegration—the process where the bone fuses with the implant—during the critical first year.
Furthermore, components are subject to immense biting forces. A higher-predictability plan accounts for the long-term support of these parts, ensuring the system can be serviced or adjusted years down the road without requiring a total redo.
The “Safeguard” Checklist: Identifying High-Risk Indicators
The process used to arrive at a cost is a more reliable indicator of satisfaction than the cost itself. Use this checklist to identify if a clinic is prioritizing your safety or simply high-volume throughput.
1. The Absence of 3D Diagnostics
If a provider quotes based solely on 2D X-rays, they are missing critical information. Without a 3D Cone Beam CT scan, a clinician cannot see the exact bone width or nerve pathways. Skipping this step shifts the risk of “anatomical surprises” onto you.
2. The “Quote Before Context” Red Flag
If a facility provides a firm quote before a specialist has physically evaluated your bone health, they are treating surgery as a commodity. A safe decision is built on your personal data, not a standardized sheet.
3. Urgency-Based Incentives
If you encounter pressure to decide quickly—such as discounts that expire or “limited-time” pricing—it indicates a business model prioritized over a clinical timeline. Biological healing cannot be rushed, and neither should your decision.
Restoring Control and Normalizing Research
You are in total control of the timeline. The “price anxiety” you feel is a signal that you lack sufficient information to feel safe.
Normalize the research phase. It is perfectly acceptable to stay in a state of “not deciding” until the logic of the clinical plan outweighs the fear of the expense. Frame professional consultations as clarification sessions, not commitments. You are gathering data to see if a provider’s approach to risk management aligns with your priorities.
The Value of Clarity
Confidence is the byproduct of clarity. When you stop asking “What is the cost?” and start asking “How are you managing the risks specific to my jaw?”, you move from a position of vulnerability to a position of power. You transition from being a consumer trying to “buy” an outcome to an informed patient selecting a clinical partner.
Reassurance and Decision Safety
Making a significant change to your dental health is a process that deserves your time. The safety of your decision is found in your comfort level with the information provided. By focusing on the how and the why of the clinical plan, you create a foundation of safety that no amount of marketing or standardized pricing can replace.